The Hidden Link Between Burnout and Pelvic Floor Dysfunction
How Stress, the Nervous System, and Midlife Burnout Impact Pelvic Floor Recovery
Published October 2025
Can Stress Make Pelvic Floor Dysfunction Worse?
You’re not imagining things — your pelvic floor symptoms often do get worse during stressful times. It feels unfair: leaks, back pain, and pressure are the last things you need when you’re already underwater. Even after the stressful season passes, those symptoms often stick around.
In this article, you’ll learn why stress and burnout make pelvic floor dysfunction worse, how the nervous system is involved, and what you can do to start healing from the inside out — today.
What Is Pelvic Floor Dysfunction?
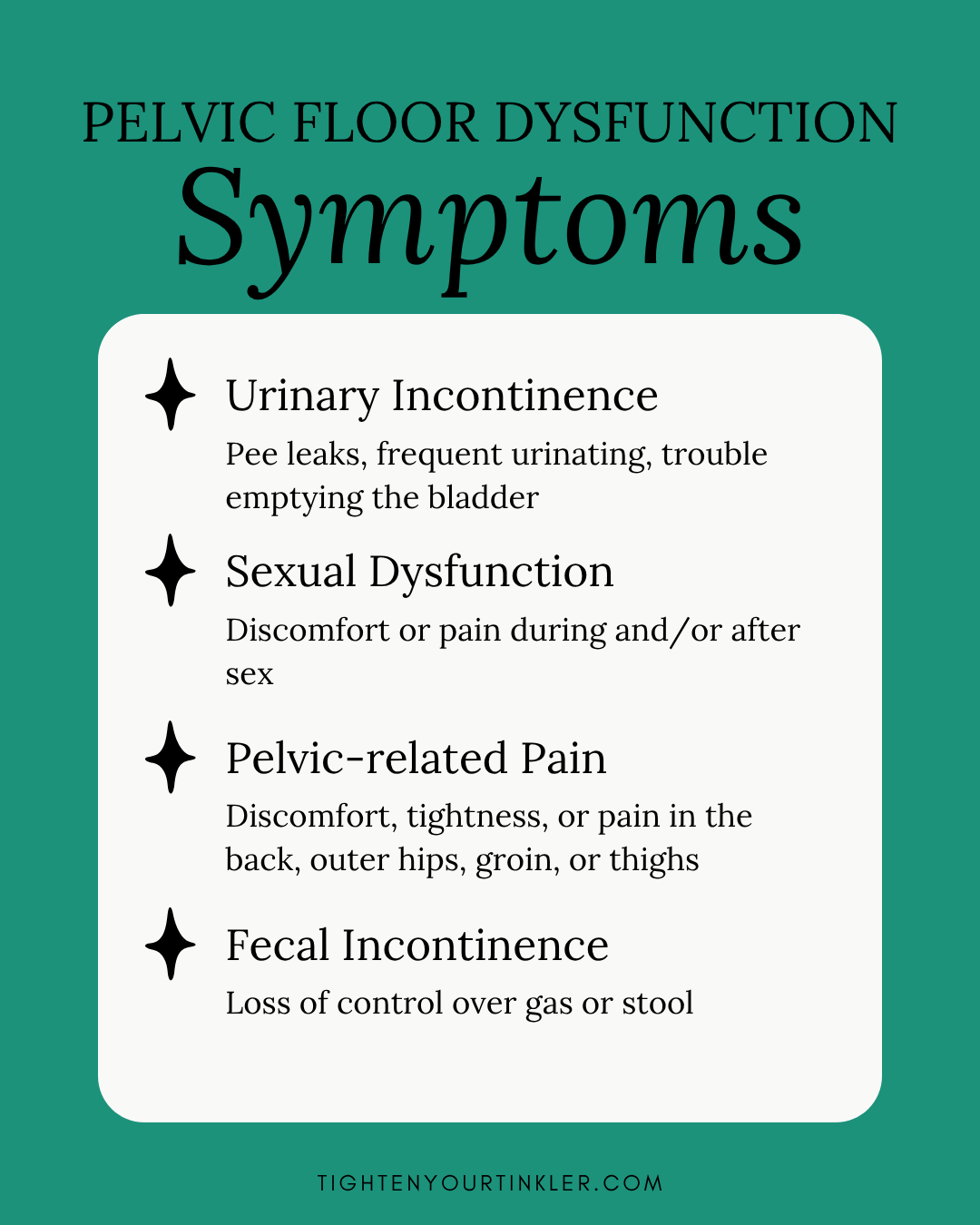
Pelvic floor dysfunction is a broad term describing several conditions that affect the muscles and tissues supporting your bladder, uterus, and bowels.
Research suggests that up to 40% of women experience pelvic organ prolapse — one of the most common types of dysfunction — where one or more pelvic organs shift due to weakened or overly tight pelvic floor tissues.
Other forms of pelvic floor dysfunction include:
-
Hypertonicity (overly tight muscles that become weak over time) — learn more about hypertonicity here
-
Diastasis recti (abdominal separation)
-
Urinary or fecal incontinence (leaks)
-
Pelvic pain, hip, or lower back pain
-
Painful sex or decreased sexual function
For this article, “pelvic floor dysfunction” refers to any combination of these symptoms.
If you’re not sure where you fall on the spectrum, our free pelvic floor quiz can help you assess your symptoms and get personalized insights.
How the Nervous System Affects the Pelvic Floor
Both Eastern and Western medicine recognize a strong connection between emotion and the pelvis — your center of gravity and, energetically, your emotional core.
Traditional Chinese Medicine links fear to the kidneys (and by extension, incontinence). Modern neuroscience now confirms that stress and trauma can be stored in the hips and pelvic region.
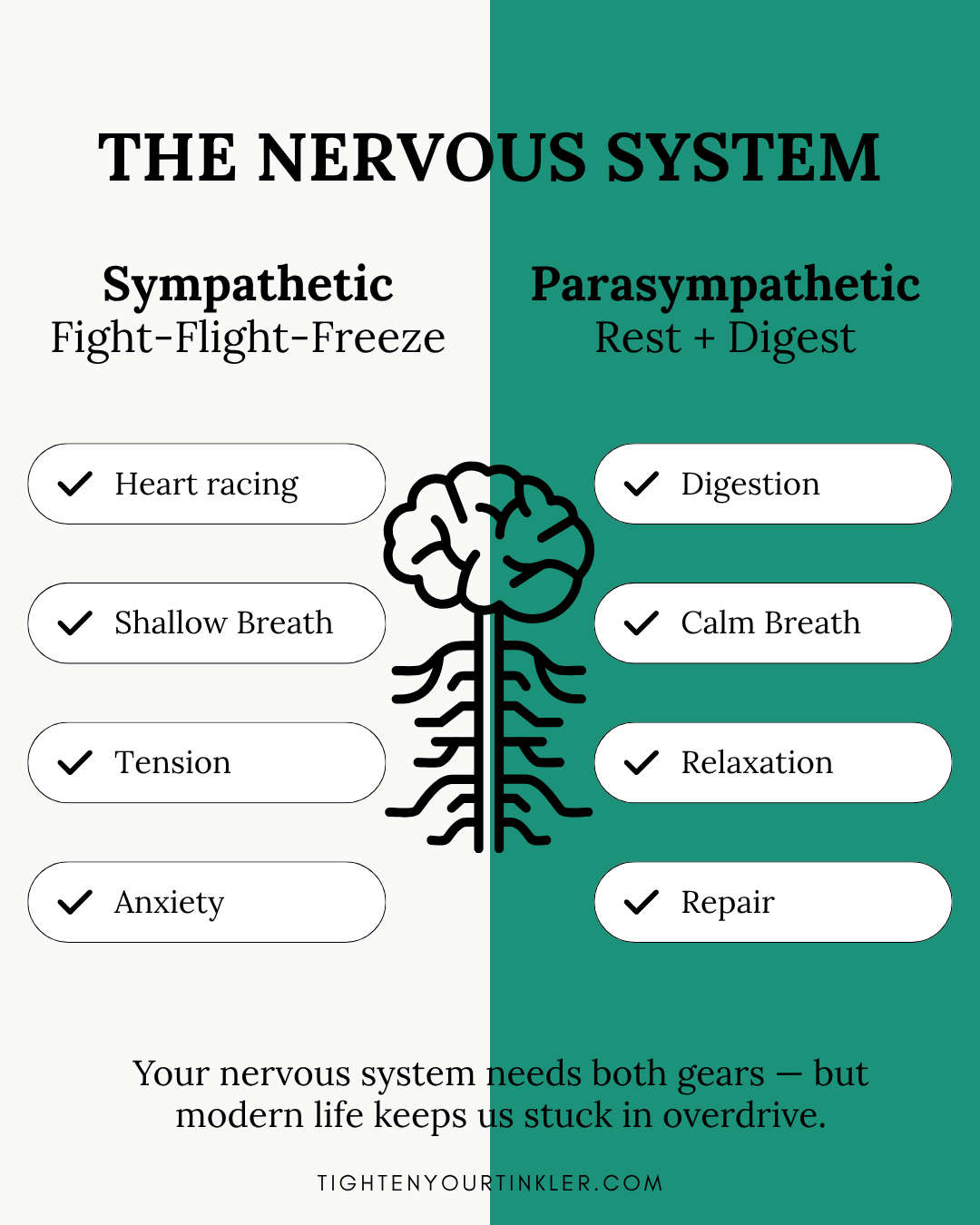
Your autonomic nervous system (ANS) controls what happens automatically in your body — your heart rate, breathing, digestion, and muscle tone. It has two main branches:
-
Sympathetic (“fight, flight, freeze”) — prepares you to react to danger
-
Parasympathetic (“rest and digest”) — helps you recover and repair
Why Modern Life Keeps You Stuck in “Fight or Flight”
In a healthy body, you move fluidly between the two states — just like a rabbit who freezes, flees, and then calmly resumes eating once danger has passed.
But modern life often traps us in a constant low-level stress state. Factors like:
-
Processed foods and nutrient depletion
-
Endless digital stimulation and screen time
-
Lack of time in nature and natural light
-
Chronic exposure to distressing news
All of these keep your stress response switched on, making it harder for your body to return to a healing state. This is called nervous system dysregulation — when your body can’t switch properly between alertness and relaxation.
Over time, this dysregulation can lead to burnout, inflammation, and yes — pelvic floor dysfunction.
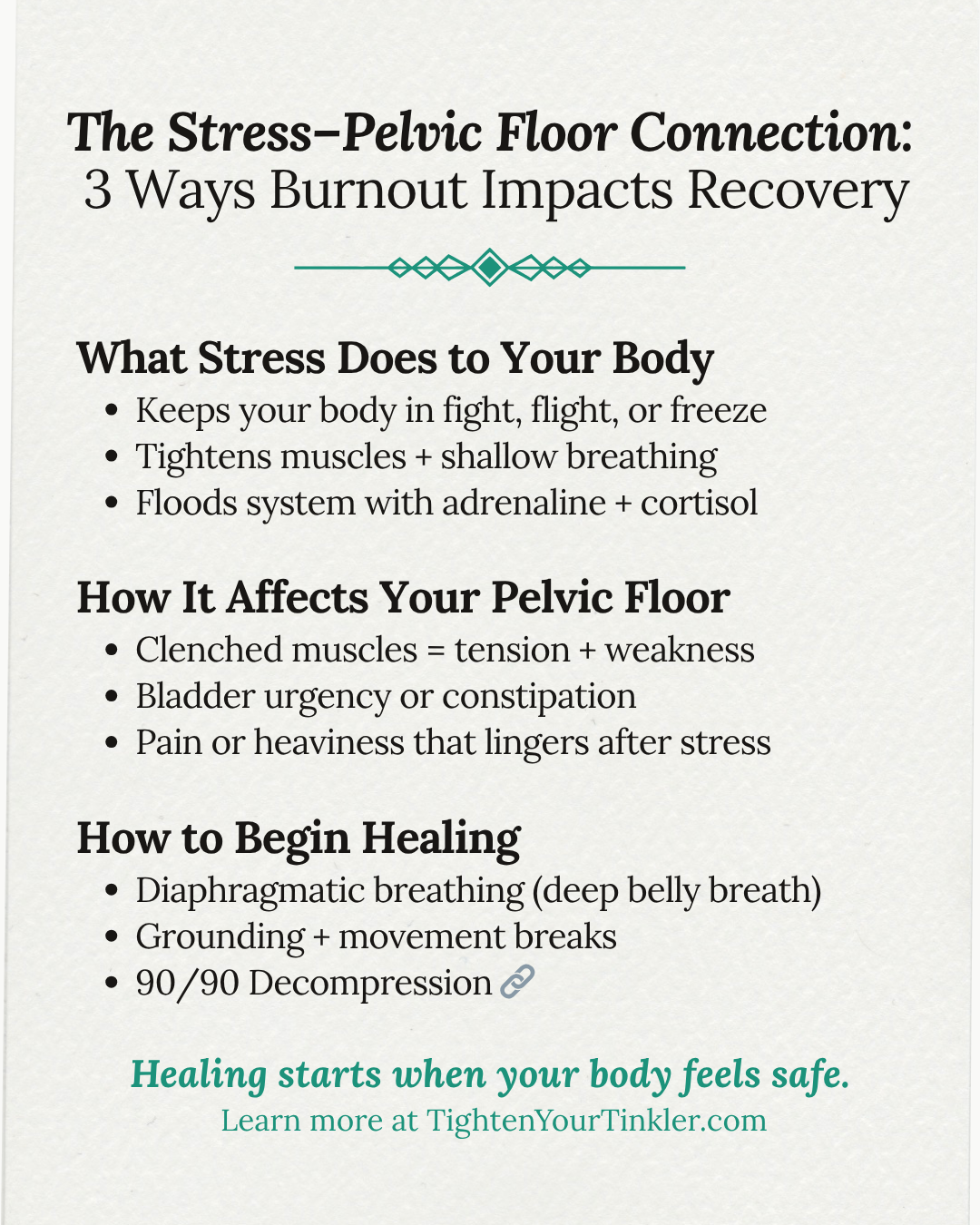
What Happens to the Pelvic Floor in Fight-Flight-Freeze Mode
When your body perceives stress or danger, the pelvic floor responds physically in three major ways:
-
Bladder constriction – Your bladder tightens, making you feel like you need to pee even when it’s not full. (“Nervous peeing” is real!)
-
Adrenaline and cortisol surges – These stress hormones tighten muscles throughout the body, including the pelvic floor.
-
Digestive disruption – Stress can cause constipation or diarrhea, both of which strain the pelvic floor and worsen symptoms.
Your body has four diaphragms that are designed to work in sync:
-
Cranial (head)
-
Thoracic inlet (upper chest)
-
Respiratory (main breathing muscle)
-
Pelvic floor
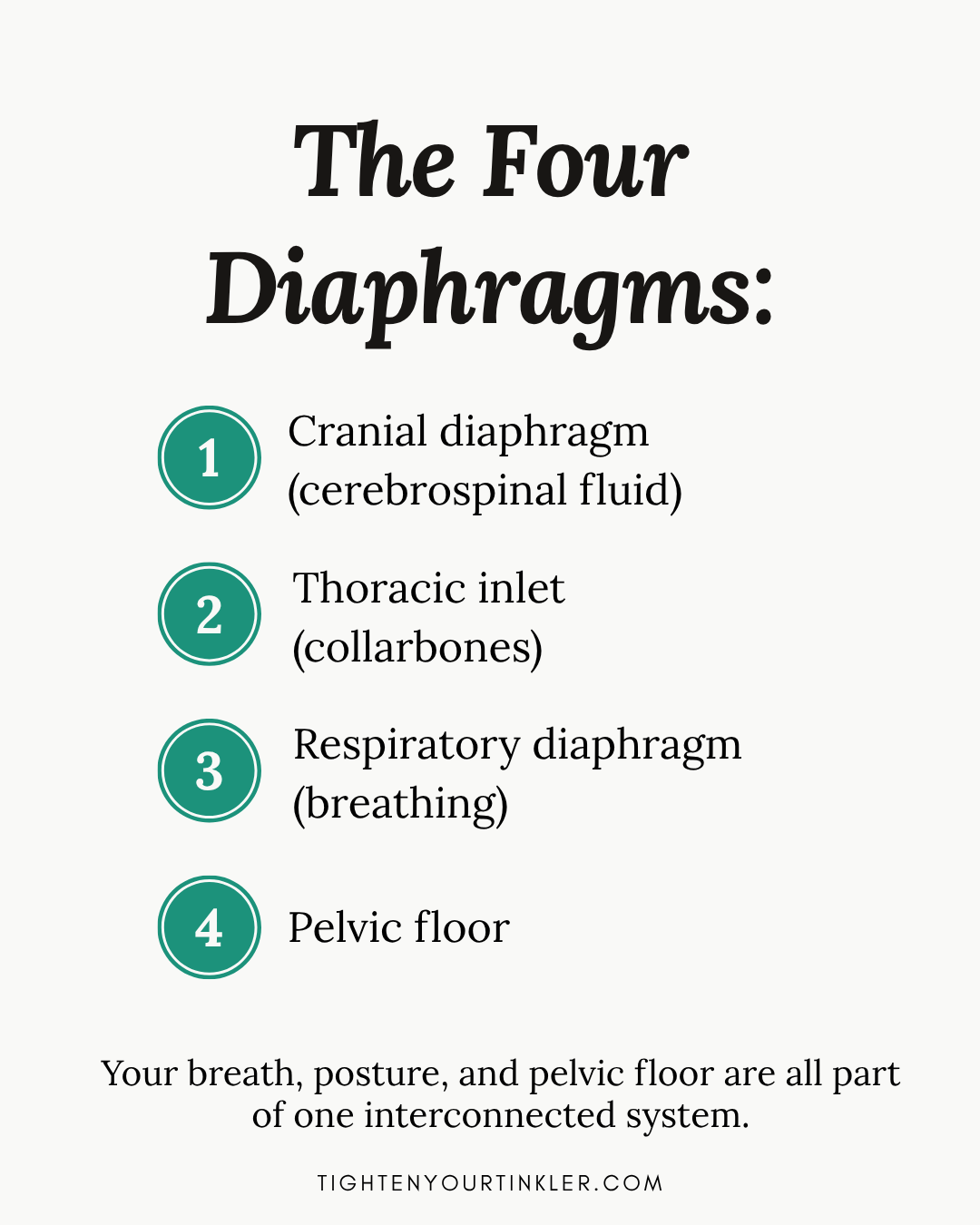
When the nervous system is dysregulated, these diaphragms lose their rhythm. Just as stress makes your breathing shallow, it causes you to clench your abs, glutes, and pelvic muscles. This can lead to:
-
Incomplete bladder emptying
-
Increased urgency or frequency
-
Recurring urinary tract infections (UTIs)
Healing Happens in “Rest and Digest”
Your body can’t heal in survival mode. True recovery — tissue repair, hormonal balance, digestion — only happens when your parasympathetic nervous system is active.
If your system isn’t shifting back into “rest and digest” naturally, you can guide it to downregulate. That’s the first step toward stopping symptom progression and restoring your pelvic floor’s function.
How to Help Your Nervous System (and Pelvic Floor) Recover
To move from fight-flight-freeze into rest-and-digest, your body needs one thing: safety.
Reducing chronic stressors is key, but you can also train your nervous system to feel safe again through consistent, gentle practices.
3 Quick Ways to Promote Relaxation and Pelvic Floor Healing
-
Diaphragmatic breathwork – Deep breathing helps reconnect the respiratory and pelvic diaphragms.
-
Grounding – Spend a few minutes each day standing barefoot outdoors or sitting quietly with your breath.
-
Meditation or prayer – These practices calm the mind and activate your parasympathetic system.
Another client-favorite is our 90/90 Decompression — a restorative resting position that eases back and hip tension while triggering a relaxation response.
👉 Watch a short demo here.
Why a Holistic Approach Works Best
Your pelvic floor isn’t an isolated muscle group — it’s part of an integrated system that includes your breath, posture, emotions, and nervous system.
This is why Kegels alone often don’t work. Real recovery requires addressing the whole body, especially the nervous system’s role in healing.
Our Kegel-Free Signature Program helps women heal their pelvic floor symptoms from home — safely, effectively, and holistically.
Key Takeaway
You can’t heal while your body still feels unsafe.
By calming your nervous system, you create the conditions your body needs to restore, strengthen, and heal your pelvic floor from within.
Where to go next:
Free Pelvic Floor Quiz ↗
Kegel-Free Signature ProgramHypertonicity Blog Post ↗
Meet Tighten Your Tinkler®️
Together, Jenn Lormand (Exercise Physiologist) and Christina Walsh (Physical Therapist) have 36 years of experience helping women heal their pelvic floors and reclaim their quality of life.
Their research-backed protocol uses movement to restore strength and function, without a kegel or Bluetooth-enabled device in sight. They’re here to share the information women need to make informed, confident decisions for their pelvic health.

Decompress your back, hips, pelvic floor (and nervous system) in just 5 minutes!
✔ No special equipment needed
✔ Free, simple, at-home position for instant relief
We hate SPAM. We will never sell your information, for any reason.